This article is adapted from a podcast featuring Kimberly Brady, HCA, BSN, RN, System Director of Care Management for United Health Services (www.nyuhs.org); Care Transitions Today, a podcast from the American Case Management Association, recently featured Kim speaking about her experience with artificial intelligence and CORTEX, now known as Dragonfly. The UHS team implemented Dragonfly in September 2018.
Background
At United Health Services Hospitals, nurse care managers are unit-based and perform utilization review (UR) and discharge planning. Due to the administrative nature of UR, they spent much of their day on utilization review rather than developing a patient-centered discharge plan to prevent readmission. In addition to the observation rate, both denials and length of stay were increasing. The nurse care managers spent three to four hours per day performing medical necessity reviews.
If the nurse care manager reviewed “patient Jones” at 9 AM and decided the patient was observation and a pending troponin came back at 11 AM, the nurse care manager would not know unless they went back into the patient’s medical record. This lack of visibility meant the opportunity to upgrade the patient faded until the next morning. We partnered with Xsolis to tackle this work, smarter.
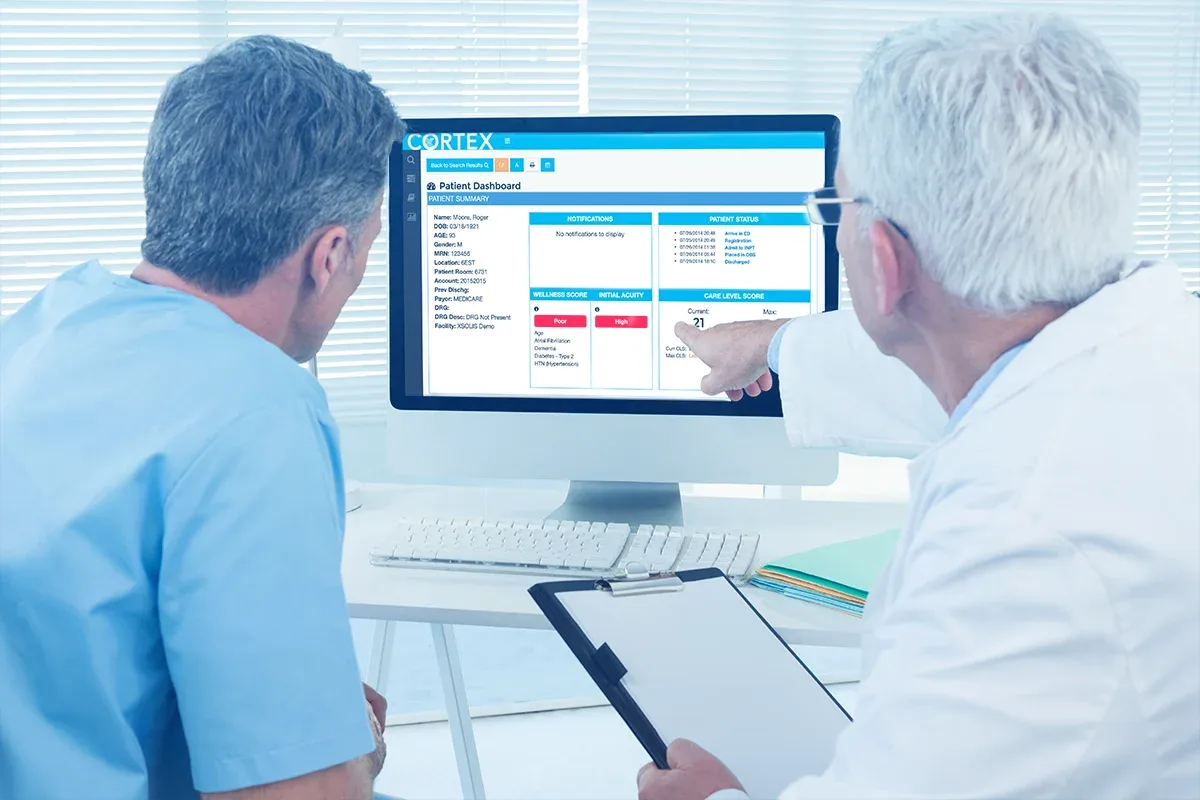
Implementing Xsolis’ Dragonfly Utilize, an artificial intelligence platform, turned our manual process into an automated process. Dragonfly Utilize generates a Care Level Score™ (CLS™) [a predictive, AI-driven view of medical necessity] for each patient with a continuous review being performed by artificial intelligence to drive action. The nurse care manager now stratifies reviews by risk from within the Dragonfly platform, allowing us to manage risk or capture opportunity.
Previously, the nurse care managers would print out a census and start at the top. Now nurses identify patients with a high Care Level Score [the higher the score, the greater likelihood of inpatient status] that are in observation that should be appropriately upgraded to inpatient; conversely, they now catch inpatients with a low Care Level Score that should be in observation. Using Dragonfly allows the nurse care manager to selectively review a subset of high-risk patients and saves utilization review resources. It also allows the nurse care manager to spend more time with the patient.
Within two days of implementing Dragonfly, my nurse care managers felt they had about ninety minutes back in their day to spend with patients and families to build solid discharge plans. They were able to return to the bedside to see and talk with patients. This has allowed them to become better nurse care managers, better clinical thinkers, and more patient-focused. They can concentrate on developing care transitions to optimize the patient’s self-care and quality of life.
We also experienced a financial benefit to the organization and a tangible benefit to the patient after implementing Dragonfly. The system’s observation rate decreased because we were placing the patient in the correct status. In addition, patients requiring a skilled nursing facility that had traditional Medicare were able to access their benefit for rehabilitation services.
Implementing Dragonfly has improved the patient experience and employee satisfaction. An additional benefit that I did not anticipate was the increase in time the nurse care manager can talk with patients and families, which increased job satisfaction. In addition, the Care Level Score generated by Dragonfly has helped to risk-stratify patients, add focus to patient care, and give staff time to offer additional services at discharge. Since COVID-19, we were able to realign resources: the utilization review process no longer fell to the nurse care managers, giving them more time for intensive patient care; we can also have two UR nurses cover nearly 300 patients due to the efficiency Dragonfly offers.
Outcomes
• Improved nurse care manager satisfaction
• Decrease in observation rate, appropriately and compliantly
• Improvement of about $1.1 million in revenue per month
• The ability to round on each patient daily by the nurse care manager has improved patient safety by having a consistent nurse assessing the patient each day
But the best result?
Better case managers, better clinical thinkers, a greater patient focus.
To hear a conversation with Kim about this approach, listen here.