Frictionless Healthcare Is Possible
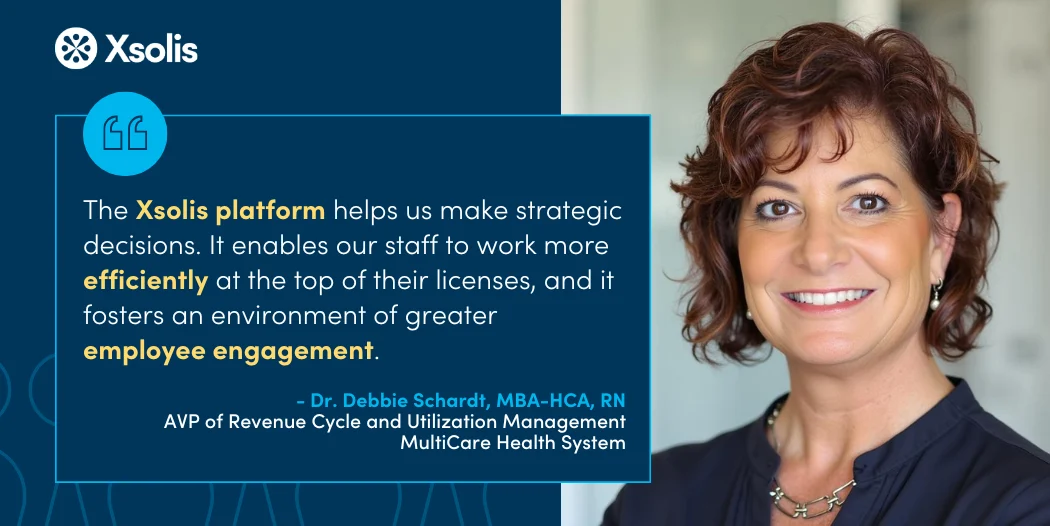
Our clients are leading the way to realize efficiencies in healthcare
A new standard is set for communication and alignment between healthcare providers and payers. Xsolis’ approach leverages artificial intelligence, proven machine learning, and data science to automate and streamline decision-making throughout the care continuum.
By facilitating data-sharing and actionable insights, healthcare organizations utilizing our solutions reduce friction and achieve optimal outcomes.